According to the American Cancer Society, 1 in 8 women in the United States will develop breast cancer.
In the spirit of this year's Breast Cancer Awareness Month, West Michigan Woman's Wine & Wig raised $46,000 to support Susan G. Komen Michigan, American Cancer Society, Gilda's Club Grand Rapids and Van Andel Institute in their fight against breast cancer.
Imagine if every month was Breast Cancer Awareness Month.
In reality, it should be.
Women and men alike should know the signs, symptoms and risks of breast cancer—and continuously check their body for signs that something is wrong.
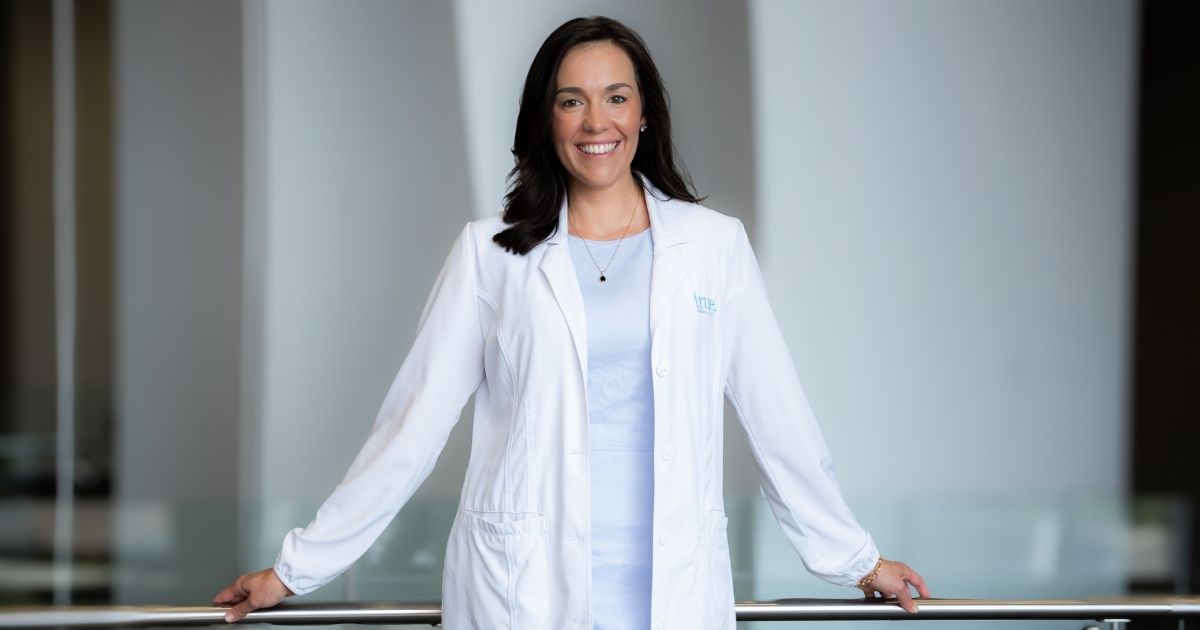
We spoke with Dr. Judy Smith, chief of the Spectrum Health Cancer Center, on how individuals could take action to detect and prevent breast cancer.

When should women begin to start checking their breasts, and how often?
Women shouldn't ever begin to start checking their breasts. They should always know what their own personal breasts feel like. Very early on, as you wash and shower, you should get to know your own body. Not just your breasts, but your whole body.
It's a continuous process. Monthly self-exams are fine, but you really want to be constantly aware of changes in your body that may alert you to something that may be going wrong.
You also need to know your risk. Talk to your primary care physician or your OB/GYN and determine whether you are at normal (average) or high risk of developing breast cancer. If you are high risk for breast cancer, everything changes. You need to be screened early and frequently.
How do women check for breast cancer? What should women look for?
Know what your breasts feel like—before you have a period, during your period, after your period, into menopause and beyond. Know what "normal" is for you. "Normal" can change over time and monthly variations can occur into menopause, particularly if you choose hormone replacement therapy. During your period, your breasts can swell, develop lumps and be painful or tender. This is normal and can also occur if you take hormones or birth control pills. As you age, breasts change and will feel different. They often become less firm and have more fatty tissue; breasts can also change when you gain weight or lose weight.
Once you know what is "normal" for you, look for new nodules or lumps in your breasts or even under your armpit. Also be alert for any unexpected change in the skin or nipple—dimpling of the skin; a nipple that turns inwards; bloody discharge from the nipple; or skin changes such as ridges, redness or scaling. Remember: Even when you find a change, it usually isn't cancer—but don't take a risk. Get it checked out by your primary care physician if it persists for more than two weeks, or is rapidly getting worse.
According to the American Cancer Society, about 2,470 new cases of invasive breast cancer will be diagnosed in men. How is breast cancer in men found? How do men check for breast cancer, and how often?
Male breast cancer is usually found on examination when men notice something is different—most often a lump in the breast tissue. Men have a tendency to ignore this as they often don't think about breast cancer. This is very dangerous. If they feel a lump, they should go to their primary care physician right away.
Don't think you can't get breast cancer just because you're a man.
What causes breast cancer?
Breast cancer is caused, like other cancers, by a series of genetic mutations, or repeated damage with in a cell. Your body typically is able to repair most of the damage, but not always. It takes about six mutations before the damage is severe enough to make a normal cell turns cancerous.
Normal cells grow and reproduce in a controlled fashion; cancer cells are out of control. When this happens to one of the types of cells that is specific to the breast, it is called breast cancer. It can take many years before a cancer cell can grow large enough to be detected by screening or show up on X-rays.
These mutations can occur by chance—bad luck—within a cell, be inherited, or be due to lifestyle or environmental factors. Cancer is thought to be often a combination of several of these factors.
What increases the risk for breast cancer?
- The biggest risk factor of all is simply being a woman.
- The second is age. The older you get, your risk increases.
- Personal history of breast cancer.
- Family history of breast, ovarian or even prostate cancer may increase your risk.
- BRCA1 and BRCA2 inherited gene mutations. It is thought that 5 to 10 percent of all breast cancers are truly inherited or passed down from your mother or father. Inheriting the BRCA1 or BRCA2 gene is a major risk factor for both men and women for the development of several types of cancers, including breast cancer. But remember, not all individuals with these genes develop cancer.
- Lifestyle is also another piece of it. Obesity, lack of exercise and excessive alcohol use may increase your risk.
- Dense breasts. Dense breasts are something only seen on mammograms and does slightly increase your risk of breast cancer. Fibrocystic changes—the nodularity you feel as you palpate or do your breast self-exam—is not the same as dense breasts. Just because you have fibrocystic changes doesn't mean you have dense breasts. They are two very different things.
- If you are younger when you have your first period, older when you have your first child, or older when you have menopause you have an increased risk.
- Radiation treatment to the chest as a child, in both men and women, can be a risk for breast cancer.
Many things can increase your risk but remember: Just because you have a risk factor doesn't necessarily mean you're going to get cancer.
What can men and women do to lower their risk of developing breast cancer?
There are certain things you can do.
First of all, know your risk. Know your family history. If you are above average risk, make sure you understand what your options are. It will likely be a combination of things.
For people who have a strong history of family breast cancer, it's important to know that in your 20s and start talking about what your options are. Cancer can occur very, very early in people who have an inherited disposition to cancer—but there are options to lower your risk. It may be that you should be tested for BRAC1 and BRAC2, or other new genes we look for.
For anyone at high risk, your provider may recommend earlier and more frequent screenings, or even preventative treatment.
For those who are at average risk, or only have one or two of these factors, the best thing they can do is try to lower the risks that are in your control. Maintain a healthy lifestyle. Try not to become overweight. Try to exercise regularly. If you drink alcohol, drink in moderation.
Know your own breasts and get your screening. Although screening does not prevent breast cancer, it does allow us to catch it early when it is most treatable. That is extremely important. The outcomes are much better the earlier you find it.
Is there anything you'd like to add?
The one thing we do know about breast cancer is that, in most women, we never can identify an exact cause. Most of us have lived our lives imperfectly. Maybe drank a little too much, or our weight's not perfect, or we didn't always exercise. We do our best—but if breast cancer does happen to you, it is highly unlikely that this is something that you could have prevented.
We almost never can pinpoint an exact cause of breast cancer. Take it easy on yourself. Try to live a healthy life. Make sure to get screened, and don't be afraid of finding out what that lump is—whether it's in the breast or somewhere else. The most important thing is to treat it early and well, with the best team available.
Bad luck is thought to be a real part of why some people get cancer and others don't. We have to do the best we can. The key is to know your breasts, know your risk, try to decrease your risk and get screened.
Courtesy of West Michigan Woman.
Photo of Dr. Judy Smith Courtesy of Kelly Braman Photography.
Save the date for next year's Wine & Wig: October 13, 2018, at the Grand Rapids Art Museum!